Overview of PNH
Paroxysmal Nocturnal Haemoglobinuria (PNH)
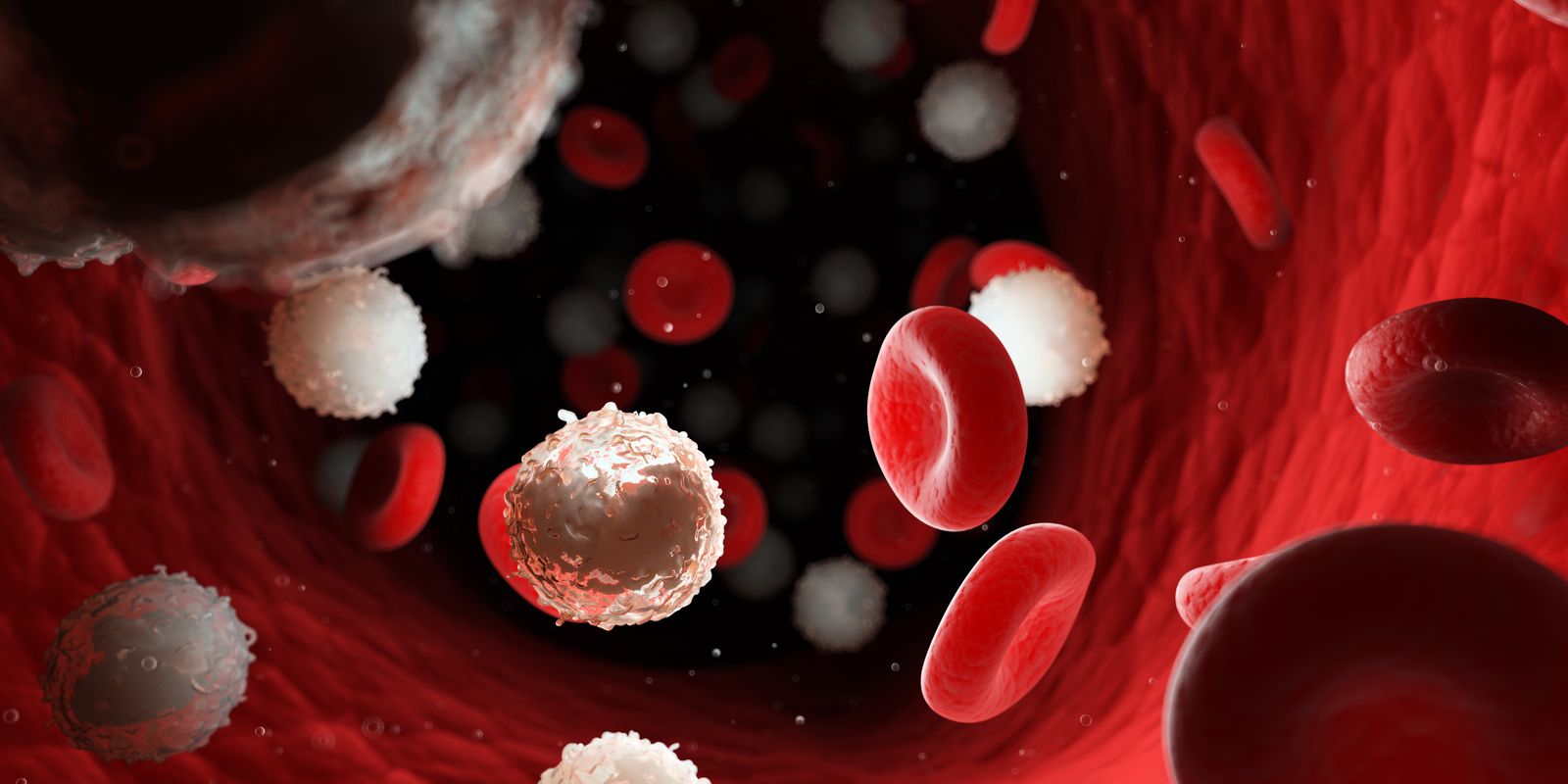
Paroxysmal Nocturnal Haemoglobinuria (PNH) is an acquired disease, characterised by intravascular haemolysis – the breakdown of red blood cells within the circulation, not in the spleen or liver, thrombosis and is associated with bone marrow failure, such as Aplastic Anaemia or PNH. PNH can occur at any age and in most patients will persist for the remainder of the patient’s life.
PNH occurs due to a clonal expansion of abnormal haematopoietic cells that are exquisitely sensitive to the uncontrolled activity of terminal complement. This occurs in the background of bone marrow dysfunction.
PNH Complications
In its most severe form, PNH leads to severe Anaemia, with patients frequently being transfusion dependent for many years (if not indefinitely).
In addition to the Anaemia, patients suffer from the direct effects of intravascular haemolysis which results in the absorption of nitric oxide, a key molecule in homeostasis, leading to smooth muscle dysfunction, platelet activation and other consequences. It can also contribute to many of the complications seen in PNH such as thromboses, renal impairment and raised pulmonary pressures.
Patients with PNH have an increased risk of blood clots (thrombosis)
We now have very effective treatments for PNH, where before these were unavailable. Approximately half of patients suffer from thrombosis, often in major vessels, and historically a third of patients die as a direct result of thrombotic complications. In addition, the haemolysis in PNH results in renal impairment in over half of patients and approximately half of patients develop raised pulmonary pressures.
PNH can occur at any age and in most patients will persist for the remainder of the patient’s life.
Approximately half of patients with PNH die as a direct result of their disease, many others are transfusion-dependent for decades and for most patients with haemolytic PNH the disease has a major impact on the patient’s quality of life. Pregnancy is extremely high risk in PNH with reported maternal mortalities of up to 20%, predominantly resulting from thrombotic complications, and reports of a high incidence of foetal loss.
Most of the observed symptoms and complications are due to the uncontrolled activity of complement on the abnormal PNH cells.
Eculizumab is a monoclonal antibody that blocks the activation of terminal complement and was approved for the treatment of PNH in 2007. Eculizumab stops intravascular haemolysis in PNH, rendering most patients’ transfusion independent whilst causing a dramatic improvement in quality of life. In addition, Eculizumab stabilises or improves renal function, prevents the occurrence of thrombotic complications and reduces the risk of pulmonary hypertension. Eculizumab has been shown to prevent most of the complications of PNH and significantly improves survival.
Ravulizumab works in a similar way to Eculizumab but remains in the body for longer, so it only needs to be administered every 8 weeks. It has been shown in clinical trials to be as effective as Eculizumab. Pegcetacoplan has been approved for treating patients that remain Anaemic on either Eculizumab or Ravulizumab. Clinical trials have shown a benefit for this group of patients.
